Hi friends!
It’s been a long while since I’ve graced this blog. So long in fact that I came to update my website (go look, I have a clinical supervision page now, yay!) and found this draft I had written in April 2020!!! I was very much pregnant with my pandemic baby then and clearly having lots of feels.
I reread my words and tears filled my eyes as I was brought right back to that time in my life. I was going to leave it as a draft and probably ignore it another 3 years, but my bestie encouraged me to let it live. So here I am publishing it as is.
It isn’t finished and you will see it abruptly ends, but hopefully doing this (+ encouragement from you all!) can give me the push to return to writing and give this beauty the part two it deserves. And not just any part two, but a part two as the me I am now. One that has survived so much more in such a strange hot world. It will be interesting to see what falls to paper on the other side. Stay tuned!
April 9, 2020
I don’t want this to be true. I mean this is what I do for a living. Inform, educate, shift norms, change policy, improve outcomes. It literally runs through my blood. I eat, sleep and breathe educating and advocating for trauma-informed care. But then I became a pregnant person navigating the same systems I tirelessly fight to be different and hot damn were my eyes opened to the realities of how truly fucked up our treatment of pregnant and birthing people (still) is.
What exactly is trauma-informed care? Well it’s not just having knowledge of trauma. NO. It’s awareness + attuned responsiveness. It’s client-centered care. It’s informed consent. Which btw cannot happen via signing a piece of paper. Informed consent is a DISCUSSION. It’s answering questions, offering options, and letting go of your ego long enough to trust and collaborate with the human in front of you. Crazy thought, but they might know a thing or two about the body they own.
Trauma-informed care is collaborative, individualized, and FLEXIBLE. It isn’t based on standards of practice or power-based protocol. NO. It requires challenging deeply rooted, historically fucked up narratives and practices that created rules and regulations around bodies to begin with. It is an investment in yourself and other humans. And more than anything it means facing your own bias, traumas, and discomfort so you can do your work through a lense of compassion, understanding, and HUMANNESS.
It seems basic. Like just connect. Be human. Easy right? *insert sad/defeated/maniacal how the fuck are we still here laugh* Unfortunately, I now have additional lived experience that sucked away so much of the hope I carry around human care becoming standard. In fact, I have many lived experiences that brought me to this work to begin with.
I am a sexual assault survivor, a mental health survivor, and a generational trauma survivor fighting everyday to break cycles passed down. All of this has impacted who I am and how I navigate the world. I’ve done tremendous healing around all it, but the whole body experience of pregnancy, birth and postpartum is always like hold your horses lady, there’s more to unravel here.
Yes, to the epic surprise of my system all that ish decided to tumble into re-consciousness the moment I entered childbearing years. I simultaneously loathed pregnancy and the loss of control I felt in my body yet also fiercely loved the cells multiplying inside me, anxious and determined to protect them from the harms I had endured.
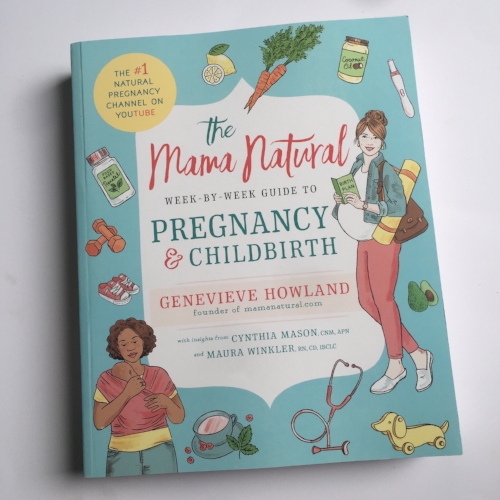
With our first, I was ready and confident in my ability to birth. I read all the books. Took the classes. We even switched providers late in pregnancy when my initial provider refused to share her cesarean stats and told me she was the expert, not me. My new doctor + doula helped me feel safe and secure again, but when it came time for labor my body perceived danger. At the time I didn’t connect my trauma history to what was happening and as a first time parent fear drove me into compliance as we navigated the policies and procedures of a hospital environment.
I was triggered by so much of the medical model of care. I had zero power and felt dehumanized as sheets were pulled back without warning. Nurses would move through the motions without asking or explaining.
Cervical checks were excruciating, my body locked in fight or flight. I sobbed and begged them not to. When they ignored my refusals and gloved up, my body would scoot away to the top of the bed, every inch of me tense with fear. They kept telling me to relax and open my legs. That I was making it worse by not being calm. No one seemed to see this scene as non-consensual or even remotely considered how this was in fact a trauma reaction being met with retraumatization. My body eventually moved into a frozen state, detached and left to relive my rape and the power it took from me.
We made multiple trips to and from the hospital, my body rigid knowing each time we returned they would force their fingers inside me again. To make matters worse my cervix was posterior so multiple nurses would enter my body in search of it’s openness. At one point they brought in the nurse with “long fingers”, two other nurses holding me down and telling me to “just relax” while her gift of length would only find my cervix still closed.
After 3 days of exhausting every trick possible, I was given the label “failure to progress”. A term I now have come to believe is actually a failure on providers and birthing spaces to create safety vs. a brokenness they dump on patients they don’t understand or find “difficult”. The term did it’s job and created a narrative in my brain that my body was in fact broken. A narrative that would follow me into my next birth and beyond.
I was determined to make my second birth different. We chose a birth center and doula. I saw a therapist. I encapsulated my placenta and we tried to make better postpartum plans (turns out these were still majorly lacking). I met all the midwives and discussed at length my trauma history, my previous birth, my potential triggers, and the needs I had in order to have a more positive birth experience.
Despite our best efforts, the system failed us. Again. I often refer to my second birth as bad luck, but no. Harmful systems don’t just magically become unharmful because you are more informed and better equipped at advocating for yourself.
The second time around my water broke to start my labor. The midwife on-call put my body on a time clock because of risk of infection. This was a new midwife for us. One that had only recently joined the practice and we didn’t know well. She clearly also didn’t know me well and ignored our preference to limit cervical checks. A practice that is even less evidence based considering my waters had broken.
After “allowing” us to labor for most of the day, the midwife wanted to check me one final time to determine if we should begin the transfer process before traffic became an issue. I had only progressed to 2-3 cm and this final check combined with the knowing I would now be forced to enter a hospital environment again sent me into a panic. Similar to my first birth, I felt outside my body, again reminded of my rape and the powerlessness that consumed me.
I could hear everyone talking in hushed tones, making a plan I didn’t agree with. Since this midwife was new to the area she didn’t want us to go to the hospital we had planned to utilize from the beginning. She had never been there and was pushing for us to go to a hospital she was more familiar with. Inside I was screaming no stick to the plan, but laboring folks can’t always verbalize the narrative happening in their brain. They are kind of busy doing a big thing. Add in the fact that I was in a trauma response and it felt as if I was a prisoner in my own birth.
Despite my internal pleas of refusal, it was off to a foreign hospital we went. I was immediately labeled “difficult”. They wanted me in a wheelchair then in the bed laying flat. I couldn’t comply with anything they requested. The contractions had gotten so intense that it felt as if I might die if I didn’t remain standing and focused. I was in survival mode. Because of my non-compliance our quality of care increasingly declined. Nurses talked down to us, reminding me frequently that I needed to stop doing what my body was instinctually doing so they could prod and poke me as the system had taught them was necessary.